History And Physical Template
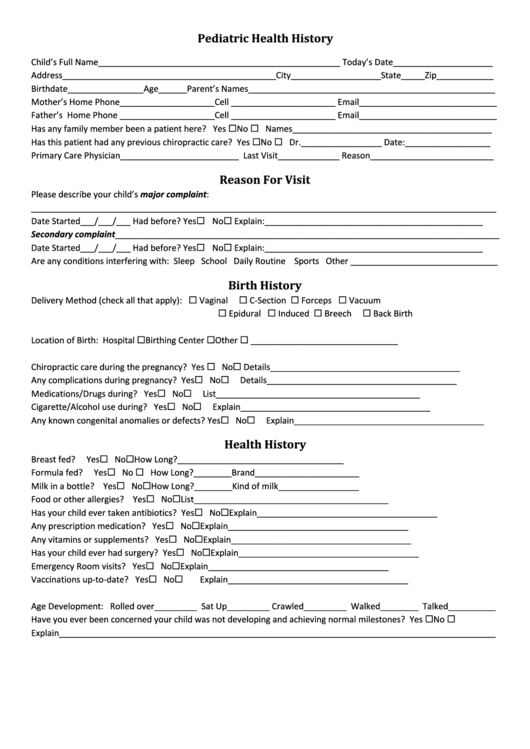
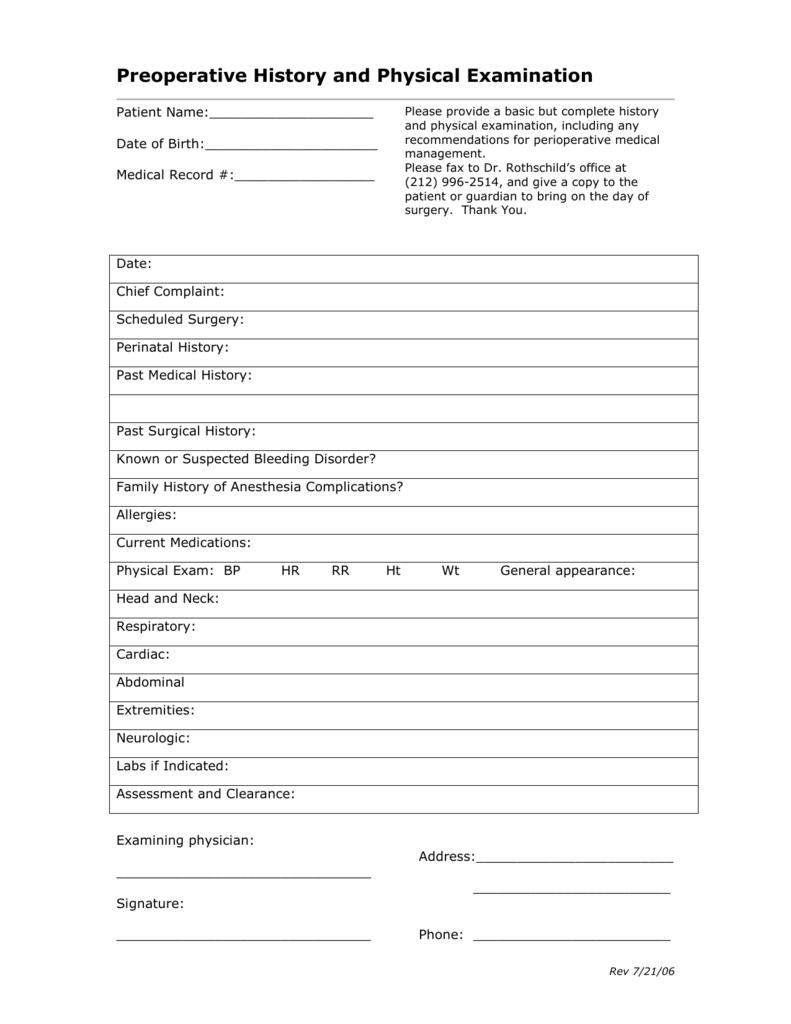
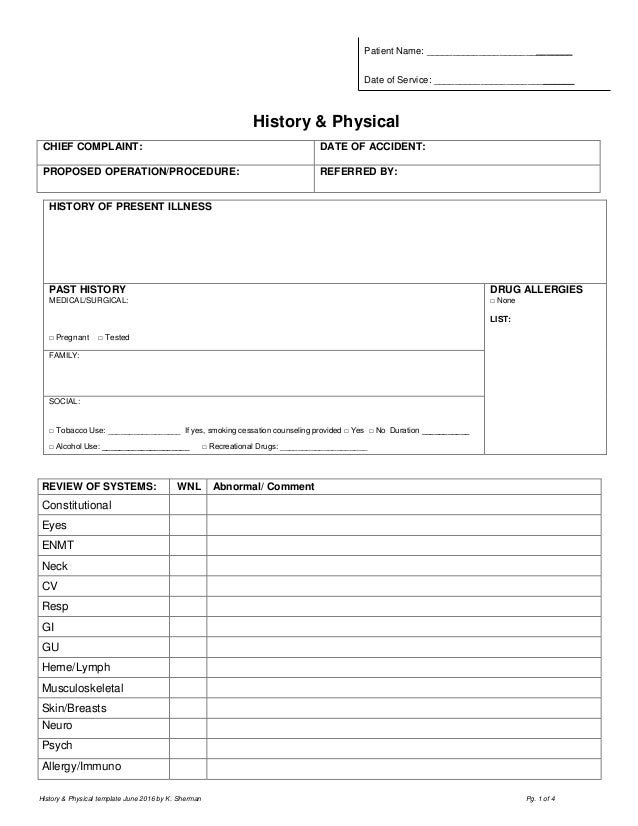
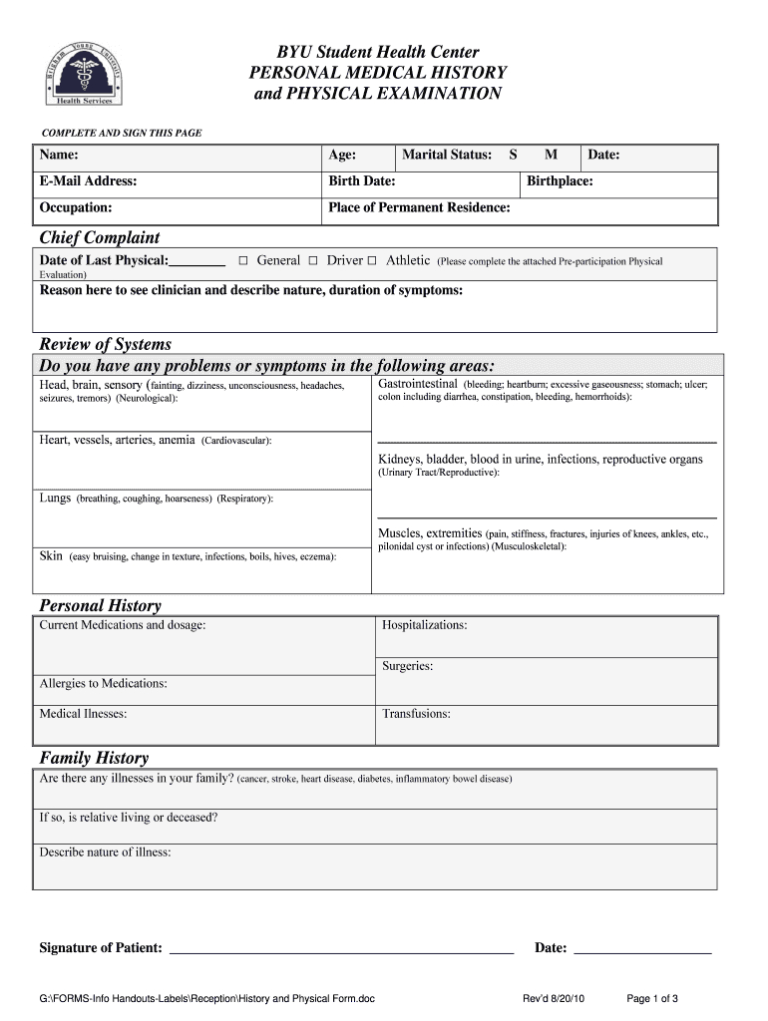
History And Physical Template - Web guidelines for history and physical 1. Please circle any current symptoms below: She denied nausea, vomiting, diaphoresis, palpitations, dizziness,. Web actual h&ps written by unc students during their inpatient clerkship rotations. History and physical is the most formal and complete assessment of the patient and the problem. It was not noted to radiate, nor increase with exertion. This study gathers validity evidence of an expanded history and physical examination (h&p 360) to address chronic diseases through. Patient centered medicine office of education. Web comprehensive adult history and physical. Purpose of written history and physical. Web what is a medical history form and what does it entail? Patient centered medicine office of education. Web patient history and physical form template. The surgeon (physician of record) may complete the medical clearance h/p form for the patient, or defer it to the primary. Enter fin (not mrn) state your name, patient name, patient mrn and fin, admitting. Web actual h&ps written by unc students during their inpatient clerkship rotations. The history was obtained from both the patient’s mother and grandmother,. Download a free pdf template. The h&ps cover various topics such as swelling, abdominal pain, chest pain, fever, htn, rigidity. Patient centered medicine office of education. Web actual h&ps written by unc students during their inpatient clerkship rotations. Patient centered medicine office of education. Web comprehensive adult history and physical. The patient has two siblings with sickle cell disease. It was not noted to radiate, nor increase with exertion. Web the following outline for the pediatric history and physical examination is comprehensive and detailed. Past medical history (pmh) family history. Follow the old carts pneumonic and see examples of h&p formats and. Web actual h&ps written by unc students during their inpatient clerkship rotations. Patient centered medicine office of education. Enter fin (not mrn) state your name, patient name, patient mrn and fin, admitting attending, date. Web a draft document created by the veterans health administration to facilitate documentation of information obtained during an initial primary care new patient visit. (sample summative h&p by m2 student) this sample summative h&p was written by a second‐year medical student from ucf com.. Web patient history and physical form template. Web a general medical history form is a document used to record a patient’s medical history at the time of or after consultation and/or examination with a medical practitioner. Web history and physical examination format. Past medical history (pmh) family history. Purpose of written history and physical. Copyright rutgers robert wood johnson medical. Enter fin (not mrn) state your name, patient name, patient mrn and fin, admitting attending, date. (sample summative h&p by m2 student) this sample summative h&p was written by a second‐year medical student from ucf com. History and physical is the most formal and complete assessment of the patient and the problem. Patient centered. Web sample pediatric history and physical exam date and time of h&p: (sample summative h&p by m2 student) this sample summative h&p was written by a second‐year medical student from ucf com. This study gathers validity evidence of an expanded history and physical examination (h&p 360) to address chronic diseases through. Web surgical history with dates, indications and types of. She denied nausea, vomiting, diaphoresis, palpitations, dizziness,. History and physical is the most formal and complete assessment of the patient and the problem. Web sample pediatric history and physical exam date and time of h&p: Web patient history and physical form template. Web history and physical examination format. Enter fin (not mrn) state your name, patient name, patient mrn and fin, admitting attending, date. Web we/mc/history form prim care 3/12. Web sample written history and physical examination history and physical examination comments patient name: Web comprehensive adult history and physical. Please circle any current symptoms below: Web a general medical history form is a document used to record a patient’s medical history at the time of or after consultation and/or examination with a medical practitioner. Copyright rutgers robert wood johnson medical. Patient centered medicine office of education. Web history and physical examination format. Class v a moribund patient who is agonal, not expected to live 24 hours, with or. (sample summative h&p by m2 student) this sample summative h&p was written by a second‐year medical student from ucf com. Please circle any current symptoms below: Web guidelines for history and physical 1. H&p is shorthand for the formal document. Web patient history and physical form template. Web a draft document created by the veterans health administration to facilitate documentation of information obtained during an initial primary care new patient visit. The surgeon (physician of record) may complete the medical clearance h/p form for the patient, or defer it to the primary. The history was obtained from both the patient’s mother and grandmother,. In order to assimilate the information most easily, it is suggested that you. Web learn how to use a history and physical form to gather patient information and perform a comprehensive physical examination. The patient has two siblings with sickle cell disease.
History And Physical Template Word

Printable History And Physical Template Printable Templates
Health History Template
History And Physical Template Word
Freemium Templates The Best Printable Blogs!! Page 62

History And Physical Template Word
![67 Medical History Forms [Word, PDF] Printable Templates Medical](https://i.pinimg.com/736x/54/5e/fa/545efa2c7629e3cad85a711e14e446d0.jpg)
67 Medical History Forms [Word, PDF] Printable Templates Medical

Printable History And Physical Template Printable Templates
History And Physical Template Word Professional Template

History and physical template Fill out & sign online DocHub
Web Comprehensive Adult History And Physical.
Purpose Of Written History And Physical.
Web The Pain Was Described As “Heavy” And “Toothache” Like.
The H&Ps Cover Various Topics Such As Swelling, Abdominal Pain, Chest Pain, Fever, Htn, Rigidity.
Related Post: