History Of Present Illness Template
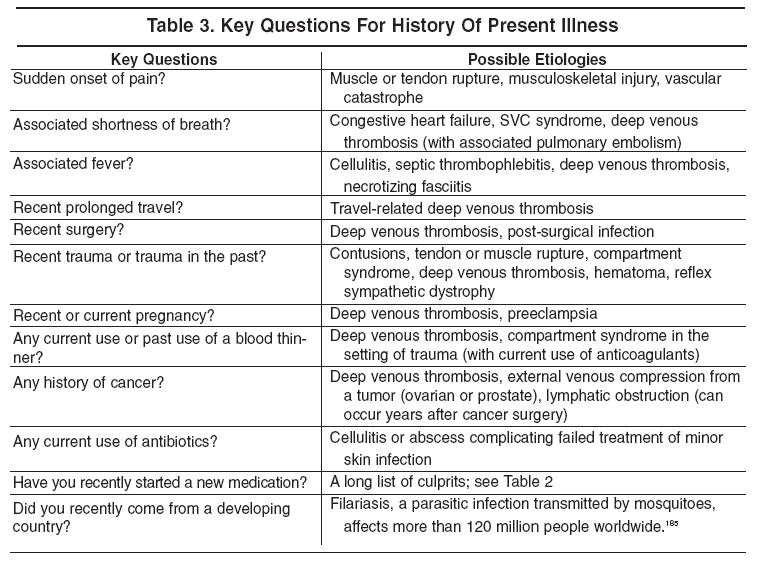
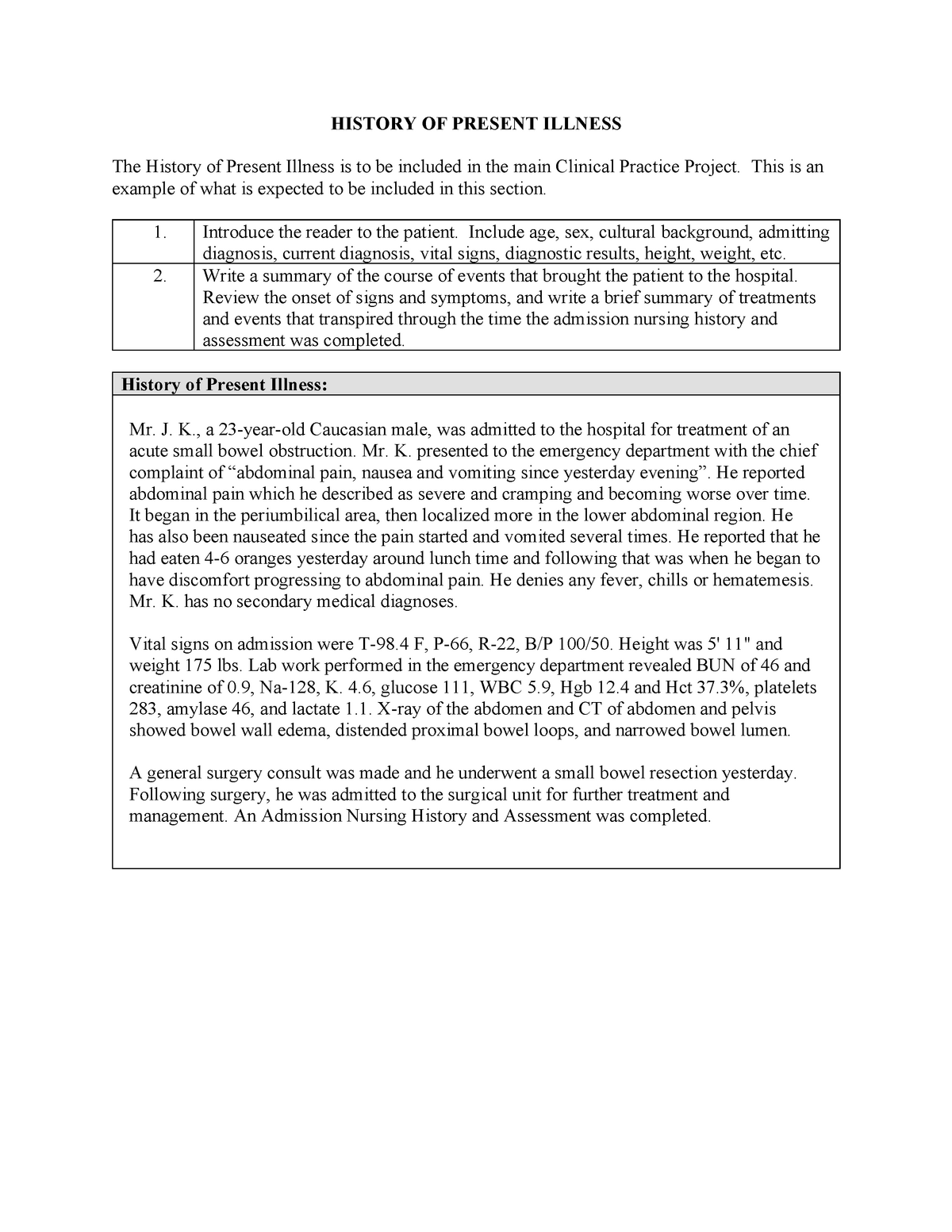
History Of Present Illness Template - Each part of the soap builds on the previous section. Please provide the date of your most recent concussion (day/month/year): Web by katreece tate. The who, what, when, where. Web history of present illness (hpi). It is a detailed set of questions designed to elaborate on the patient’s chief complaint or presenting symptom. To determine what to include in the history of present illness (hpi), keep these questions in mind. Did your concussion result in any difficulty with your memory? Web the extent of history of present illness, review of systems, and past, family and/or social history that is obtained and documented is dependent upon clinical judgment and the nature of the presenting problem(s). Web the documentation template includes the following sections: Please provide the date of your most recent concussion (day/month/year): Each part of the soap builds on the previous section. Web by katreece tate. The hpi should provide enough information to clearly understand the symptoms and events that lead to the admission. Web the documentation template includes the following sections: A large percentage of the time, you will actually be able to make a diagnosis based on the history alone. Web one such template lists four components of a medical evaluation and uses the acronym soap: This covers everything that contributed to the patient's arrival in the ed (or the floor,. Please provide the date of your most recent concussion. Web history of present illness this is the first admission for this 56 year old woman, convey the acute or chronic nature of the problem and who states she was in her usual state of good health until establish a chronology. Chief complaint, history of present illness, review of systems, sexual assault, annual screening questionnaire, and health literacy assessment. Web. An accurate history is the first step in determining the etiology of. Did your concussion result in any loss of consciousness? Web the documentation template includes the following sections: Chief complaint, history of present illness, review of systems, sexual assault, annual screening questionnaire, and health literacy assessment. Each part of the soap builds on the previous section. She came immediately to the ed b/c she was having difficulty swallowing and some trouble breathing due to obstruction caused by the swelling. Web by katreece tate. Web history of present illness: The who, what, when, where. To determine what to include in the history of present illness (hpi), keep these questions in mind. Always start with the standard questions applied to the patient’s chief concern (s): 30 day free trialfree mobile apptrusted by millionsedit on any device Web history of present illness: Web history of present illness this is the first admission for this 56 year old woman, convey the acute or chronic nature of the problem and who states she was in. Web by katreece tate. She reports that she was seen for similar symptoms previously at her primary care physician’s office six months ago. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Web the extent of history of present illness, review of systems, and past, family and/or social. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Always start with the standard questions applied to the patient’s chief concern (s): Consider saving this document electronically to quickly cut and paste sections into your ehr. Web history of present illness (hpi). Web history of the present illness: Web history of present illness (hpi) the hpi begins with a simple one line opening statement including the patient's age, sex and reason for the visit. Web history of present illness (hpi) assessment and plan template. Web the history of present illness (hpi) is also called the primary history. 77 y o woman in nad with a h/o cad, dm2,. She was first admitted to cpmc in 1995 when she presented with a complaint of intermittent midsternal chest pain. Web history of present illness: Web the documentation template includes the following sections: A large percentage of the time, you will actually be able to make a diagnosis based on the history alone. Consider saving this document electronically to quickly cut. The letters stand for onset; Web the extent of history of present illness, review of systems, and past, family and/or social history that is obtained and documented is dependent upon clinical judgment and the nature of the presenting problem(s). It is a detailed set of questions designed to elaborate on the patient’s chief complaint or presenting symptom. Web history of present illness: In the realm of medical diagnosis and patient care, a thorough understanding of the history of present illness (hpi) is paramount. Please provide the date of your most recent concussion (day/month/year): A large percentage of the time, you will actually be able to make a diagnosis based on the history alone. Web the history of present illness (hpi) is also called the primary history. Web history of present illness: Web one such template lists four components of a medical evaluation and uses the acronym soap: Consider saving this document electronically to quickly cut and paste sections into your ehr. Web history of present illness: Did your concussion result in any seizures or convulsions? Web history of the present illness: The who, what, when, where. To determine what to include in the history of present illness (hpi), keep these questions in mind.
PDF Template for The History of Present Illness USF Health Doc
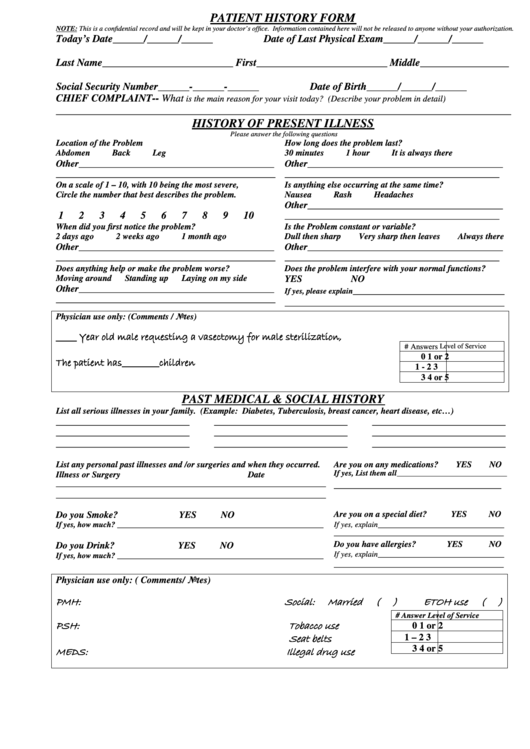
Patient History Form/history Of Present Illness/past Medical & Social
History Of Present Illness Template williamsonga.us
History Of Present Illness Template

History Of Present Illness Template History Of Present Illness Template

Fillable Online PATIENT HISTORY FORM HISTORY OF PRESENT ILLNESS Fax

PPT Clinical Documentation Tips Reflection of Acuity & Medical
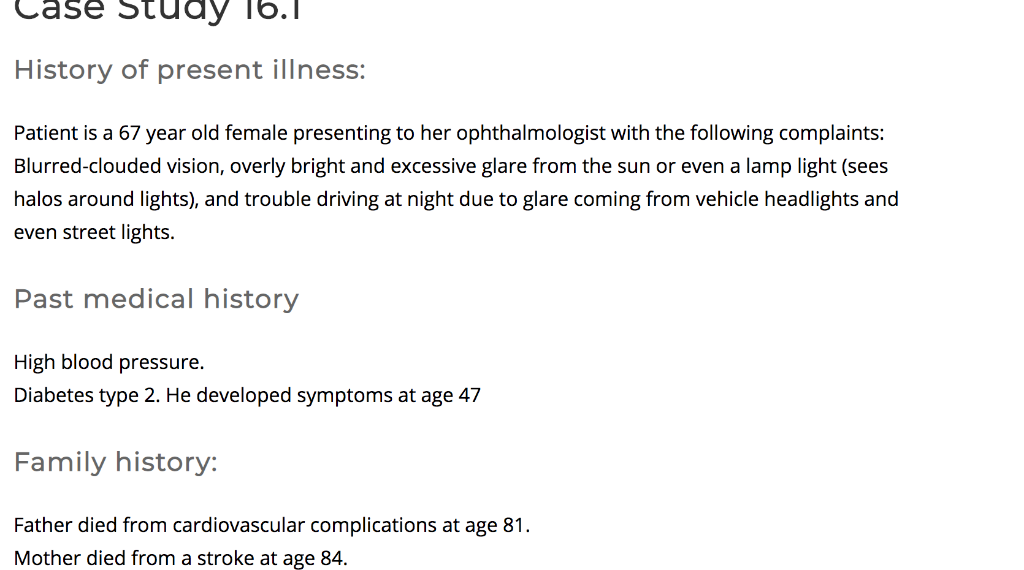
50 Best History of Present Illness Example Tips Ultimate Guide 2024

History Of Present Illness Template
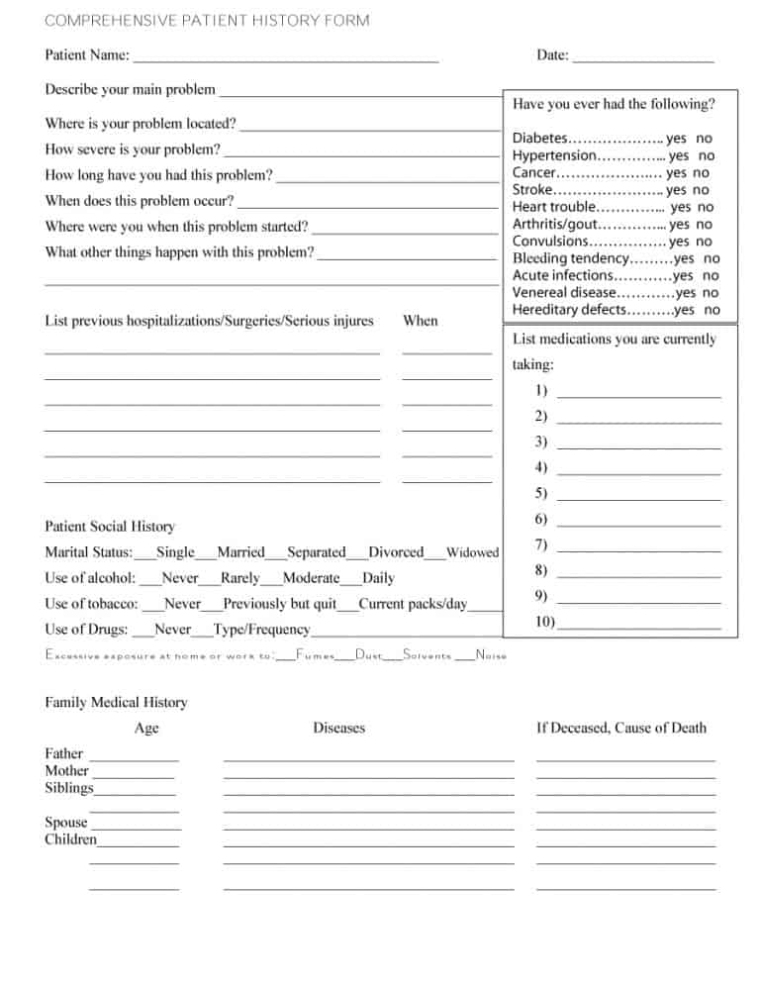
67 Medical History Forms Word Pdf Printable Templates For History Of
Web History Of Present Illness This Is The First Admission For This 56 Year Old Woman, Convey The Acute Or Chronic Nature Of The Problem And Who States She Was In Her Usual State Of Good Health Until Establish A Chronology.
Consider Saving This Document Electronically To Quickly Cut And Paste Sections Into Your Ehr.
The Soap Evaluation Is A Basic Form Of Communication That Can Be Expressed Verbally And In Written Form.
An Accurate History Is The First Step In Determining The Etiology Of.
Related Post: